
With our influenza vaccines, we seek not only to prevent influenza but also to protect as many people as possible from its severe complications, supported by the highest level of evidence.

Martin Ryser
Global Medical Affairs, Influenza & Covid
Did You Know?
Flu can wreak havoc on major organs and systems.(1-5)
Influenza can worsen symptoms of other chronic diseases and can lead to hospitalization. (2)
People under 5, over 65, pregnant, or living with chronic conditions are the most at risk of severe complications from flu. (1)

Innovating to Continue to Protect Beyond Flu
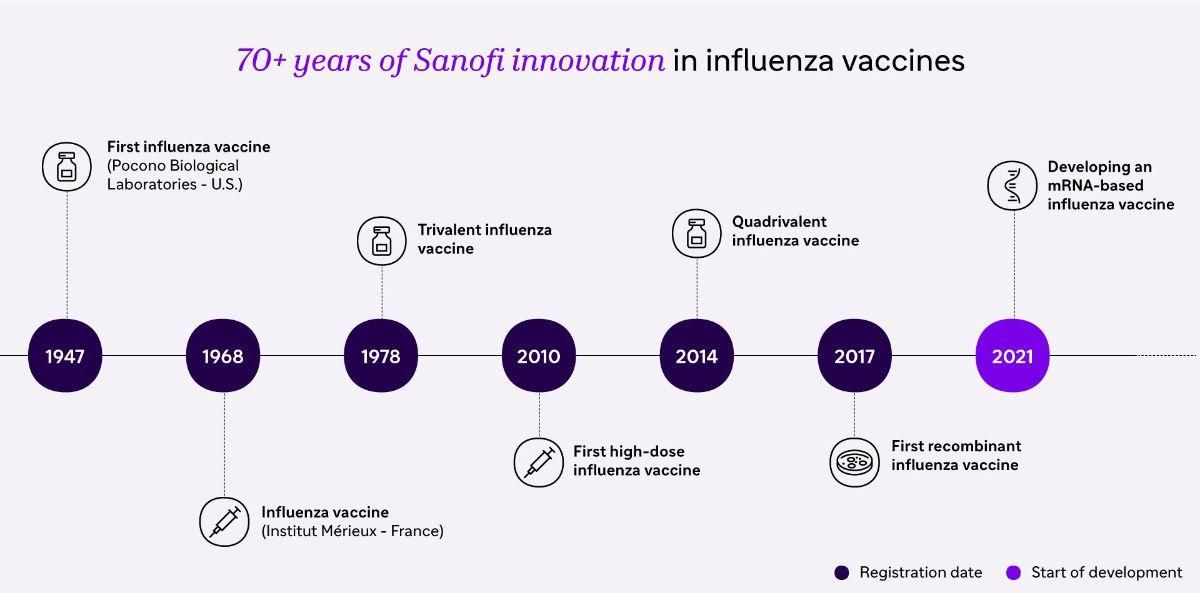
Not all flu vaccines are the same. We’re using mRNA, protein-based technologies, and novel antigen-selection methods to develop next generation vaccines, designed to induce broader protection against different strains of the influenza virus. We never stop innovating on our existing technologies, which help us protect people everywhere against flu and its complications.
The Real Burden of Flu
Flu is an unpredictable infectious disease and can be severe (2).
- Flu can cause a 10X increased risk of heart attack within the week following an influenza infection. (1)
- Flu can increase your risk of stroke and pneumonia X8 (1,5)
- Flu vaccination can reduce the risk of flu triggered heart attacks by up to 45% (6).
That’s why vaccination is so important, especially for people at increased risk of severe infection (2).
All About Flu

Defending Flu Vaccine Coverage Rates to Help Protect the Most Vulnerable
How we strive to protect against the flu.

Protecting Heart Health: Flu Vaccines and Beyond
Discover how we seek to protect every kind of heart

What Is a Flu Strain?
You’ve probably already heard about Flu Strains, but do you know exactly what it is? Let’s ask our scientists.
Explore More

Why Vaccines Matter
Redefining R&D: How Immunoscience is Driving the Pipeline of the Future
References
- Warren-Gash C, et al. (2018) Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Resp J 51:1701794; DOI: 10.1183/13993003.01794-2017
- World Health Organization (2018) Influenza (seasonal) Fact Sheet. Accessed July 19, 2024
- Andrew MK, et al. (2021) Persistent functional decline following hospitalization with influenza or acute respiratory illness. J Am Geriatr Soc 69:696-703; DOI: 10.1111/jgs.16950
- Samson SI, et al. (2021) Quantifying the impact of influenza among persons with type 2 diabetes mellitus: a new approach to determine medical and physical activity impact. J Diabet Sci Technol 15:44-52; DOI: 10.1177/1932296819883340
- Kubale J, et al. (2021) Individual-level association of influenza infection with subsequent pneumonia: a case-control and prospective cohort study. Clin Infect Dis 73:e4288-e4295; DOI: 10.1093/cid/ciaa1053
- MacIntyre CR, (2016) Influenza vaccine as a coronary intervention for prevention of myocardial infarction. Heart 102:1953-1956. DOI: 10.1136/heartjnl-2016-309983
Page updated September 2024