Vaccines: Innovation for Disease Prevention and Control
All vaccines help protect public health, but they are not all made the same way. Find out how our teams are developing vaccines with the greatest potential to fight infectious diseases.
Since Louis Pasteur first discovered the connection between micro-organisms and infection, generations of scientists have developed vaccines that train our immune systems to combat infectious diseases. We proudly embrace this legacy. Every day, our teams are pouring enormous energy and creativity into finding new ways for people to live in harmony with the micro-organisms that share our environment, while defeating those that are harmful.

Jean-François Toussaint
Global Head of Research and Development, Vaccines
For nearly 150 years, vaccines have provided high levels of protection against diseases that once ravaged entire populations. To stop infection in its tracks, our R&D teams develop vaccine antigens: molecules that help trigger the body’s immune response against disease-causing germs, or pathogens. We also explore how vaccines could be used to prevent chronic diseases and collaborate globally to help prepare society for future outbreaks.
Types of Vaccines¹
There are so many different disease-causing microbes that no single technology could tackle them all. Our teams use a wide range of tools to develop vaccines that can target proteins, sugars (polysaccharides), or other features that enable bacteria and viruses to thrive in the human body.

Live-attenuated Vaccines
Some vaccines are based on weakened whole viruses, which can help the body build its defenses without causing disease. Yellow fever has been kept in check and smallpox eradicated thanks to live-attenuated vaccines.
Inactivated Vaccines
The polio, rabies, and most influenza vaccines are based on whole viruses that have been cultured in the lab and inactivated, or killed, before they are used.

Recombinant Protein Vaccines
When only part of a pathogen is needed to create a vaccine, sometimes the right approach is to synthesize that antigen using recombinant technology. This involves producing the protein in the lab and formulating it into a vaccine. Our recombinant hepatitis B vaccine is made this way.
Polysaccharide-based Vaccines
Some disease-causing bacteria, such as Heamophilus Influenza type B, have a coating made of polysaccharides (sugars) that protects them from being destroyed by immune cells.2 Using one of these sugars as an antigen can stimulate the body to produce antibodies that target the bacteria's protective coating, effectively lowering the drawbridge for immune cells to attack. In a conjugated polysaccharide vaccine, the sugar is linked to a protein3 to make the immune response more durable.

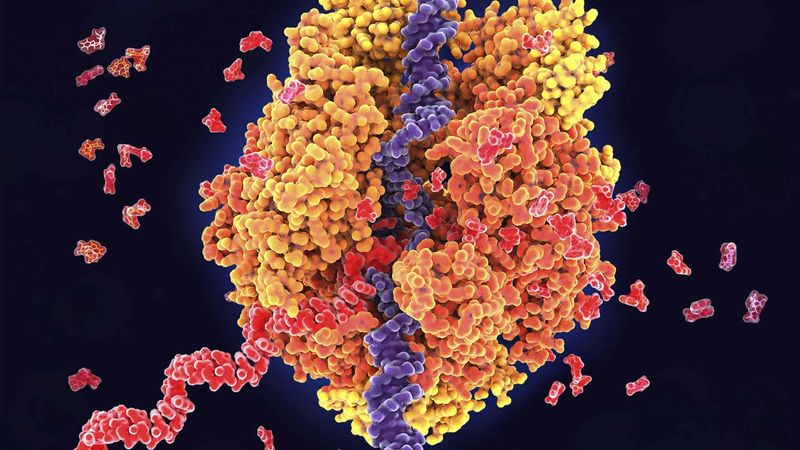
Messenger RNA Vaccines
mRNA carries genetic sequences that instruct cells to make proteins. mRNA can be designed to carry instructions for producing a viral or bacterial antigen directly to cells in the body. In an mRNA vaccine, the mRNA instructions are carefully encased in a nanoparticle, which keeps it intact until it enters its target cell. Once the cell produces the antigen, the immune system is stimulated to produce antibodies against it.
Our teams are using mRNA technology to develop vaccines against several common pathogens, such as influenza, RSV in older adults, and chlamydia.
Bridging Gaps in Immunization

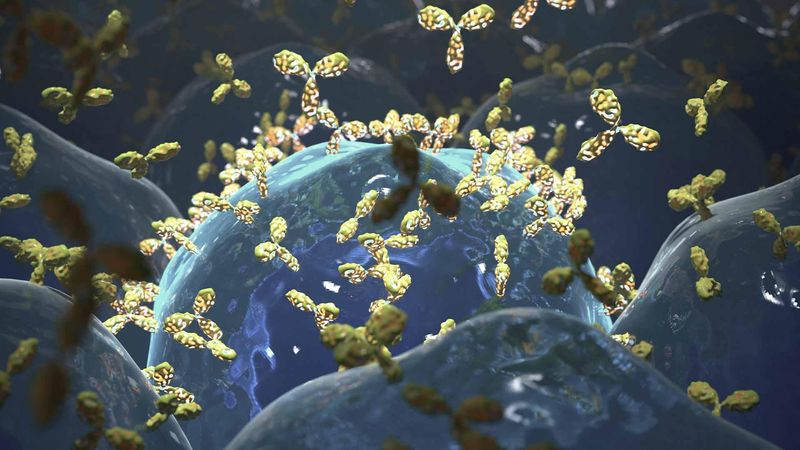
Monoclonal Antibodies
Rather than stimulating the body to produce its own antibodies, we can design monoclonal antibodies that can offer immediate protection against certain diseases. This kind of rapid protection could bridge important gaps in immunity, for example when infants are too young to be given certain vaccines, or when no vaccine is available.
Adjuvants to Boost the Immune Response
Some vaccines are a mixture of antigens and an adjuvant: a substance that boosts the immune response.4 An adjuvant can potentially increase the vaccine's effectiveness and make it protective for longer, or against multiple variants (or strains) of a virus. It can also reduce the amount of antigen needed per dose. That's how an adjuvant can help us make a vaccine supply available to more people, more quickly during disease outbreaks.
We develop our own adjuvants and work with partners to combine our antigens with their adjuvants, as we've done in the development of our COVID-19 vaccine candidate.
Data Science Helps Us Make Better Vaccines
The most important step in making a vaccine is understanding the enemy inside and out. Knowing its weaponry, its vulnerabilities, and its unwitting allies in the body helps us make vaccines that take aim at the right target. But pathogens can change. To stay ahead of them, we use machine learning and other AI techniques to collect and analyze huge amounts of information. That gives us the greatest chance of beating pathogens at their own game.
Making Immunization Easier
We're the world leader in pediatric combination vaccines: single formulations that protect children against multiple infectious diseases. Combination vaccines increase vaccination acceptance by simplifying immunization schedules,5 which helps keep community immunization rates high over the long term. Combining antigens is a complex process: each one must remain stable, intact, and immunogenic, and it cannot react with any other element of the vaccine. Our teams ensure that stability is consistent and long-lasting in high volumes of vaccines.
Protection Beyond Infectious Diseases
Many infectious diseases have been found to be linked to other serious diseases. For example, following an influenza infection, there’s a 10-times greater risk of having a heart attack and 8-times greater risk of having a stroke.6
Our goal is to design vaccines and immunotherapies that could vastly improve quality of life for people around the world. That's why we take a holistic approach to R&D, centered on the collective effects of vaccines over time. By boosting immunity regularly, we believe we can engage the whole immune system in ways that keep it running smoothly, helping people fend off both infectious and chronic diseases.
Learn More About Vaccines

What's in Our Pipeline
mRNA in Vaccines and Beyond
Vaccines and Monoclonal Antibodies in Immunization

The Upshot: Everything You Need to Know About Vaccines
References
- World Health Organization (2020) How are vaccines developed? Accessed on 16 December 2021
- Mandell LA (2012) Streptococcus pneumoniae infections. In: Goldman L, Schafer AI, Eds. Goldman's Cecil Medicine, 24th ed. 1820-1823 pp; doi: 10.1016/B978-1-4377-1604-7.00297-9
- Ahmad H, Chapnick EK (1999) Conjugated polysaccharide vaccines. Inf Dis Clin N Amer 13:133-133; doi: 10.1016/S0891-5520(05)70046-5
- Centers for Disease Control and Prevention (2020). Accessed on 16 December 2021.
- Kurosky SK, et al. (2017) Effect of combination vaccines on completion and compliance of childhood vaccinations in the United States. Hum Vaccin Immunother 13:2494–2502. doi: 10.1080/21645515.2017.1362515
- Warren-Gash C, et al. (2018) Laboratory-confirmed respiratory infections as triggers for acute myocardial infarction and stroke: a self-controlled case series analysis of national linked datasets from Scotland. Eur Respir J, 51:1701794; doi: 10.1183/13993003.01794-2017
MAT-GLB-2105625 v 1.0 | February 2022
2022-01-28