Vaccines Help Protect Us
Every year, vaccination saves up to 5 million lives around the world. But an additional 1.5 million lives could be saved with improved vaccination coverage.1
Our Vaccines at a Glance
500M+
people vaccinated annually with our vaccines worldwide.2
2.5M
vaccines doses supplied every day.2
€1bn
R&D vaccine investment annually. 2
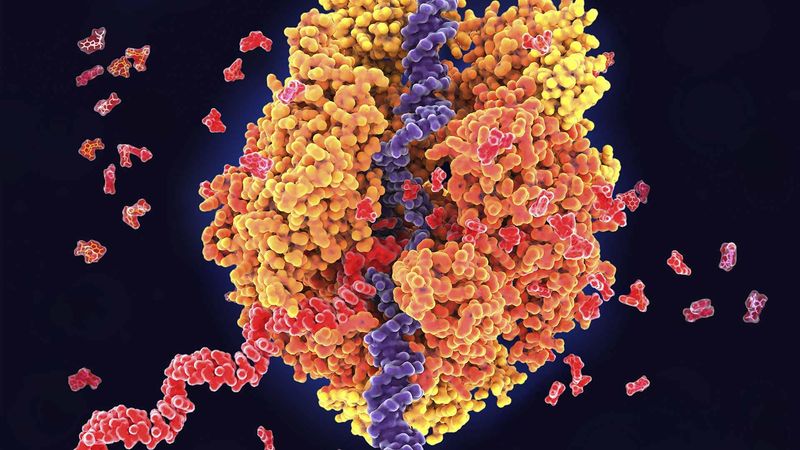
What’s Next in Vaccines?
Our leadership in immunoscience drives transformative innovation across our vaccine portfolio. This expertise underpins our cutting-edge vaccine research, enabling us to help tackle global health challenges with innovative solutions. Learn how our commitment to advancing immunoscience fuels breakthroughs in vaccine R&D.
Explore More

How We Make Vaccines
References
- World Health Organization (2019) Immunization Facts in Pictures. Accessed November 2024
- Sanofi – internal references
MAT-GLB-2200131 v3.0 12/2024