Sanofi's Multi-Front Attack on Cancer

Cancer therapy is undergoing a renaissance, as scientists across the industry pursue new ways of attacking malignant cells. We spoke with John Reed, Executive Vice President and Global Head of R&D, and Frank Nestle, Chief Science Officer and Head of Research at Sanofi, to find out how Sanofi scientists are building an R&D pipeline that addresses critical gaps in cancer care.
Our ambition has been to turn outstanding science into medicines that have the potential to transform lives, and we are beginning to see that unfold in oncology where new approaches like synthetic biology are allowing scientists to harness the immune system with greater precision than ever before. It is incredibly exciting to see Sanofi’s pipeline expand as our teams embrace new technologies and apply their deep understanding of disease biology to develop the medicines of the future.

Paul Hudson
CEO
How are Sanofi scientists overcoming oncology's most significant challenges?

John Reed: At Sanofi, we are committed to building the next generation of innovative molecules that either directly attack and destroy cancer cells, or that harness the power of the immune system to encourage the patient’s own self-defense mechanisms to eradicate the cancer. Our foundations for fighting cancer are reinforced by the diverse toolbox of technologies we have been assembling for designing new types of medicines. A lot is known already about cancer biology but many of the defects are not so easily fixed.
The more “weapons” for attacking cancer we stock in our armory, the more opportunities our scientists have for discovering therapies that are effective for patients.

Frank Nestle: One major factor driving innovation at Sanofi is the interplay between immuno-oncology and molecular oncology. Our molecular oncology teams harness revolutionary chemistry to develop drugs that target intracellular proteins in cancer cells. One example is an investigational molecule that targets estrogen-receptor alpha in breast cancer cells. This oral selective estrogen receptor degrader (SERD) flags disease-causing proteins for disposal–an approach that points to new possibilities for treating hormone-receptor-positive breast cancer.
John: But while our scientists can sometimes conquer a cancer-relevant target using small-molecule chemistry approaches, we need a variety of tools to tackle cancer. Take, for example, what we are currently exploring with interleukin-2 (IL-2). IL-2 is a promising molecule for cancer immunotherapy that stimulates immune cells to fight cancer, but also has toxic effects. To tame IL-2, we are reaching into our toolbox to pull out the SYNTHORIN™ synthetic biology platform.
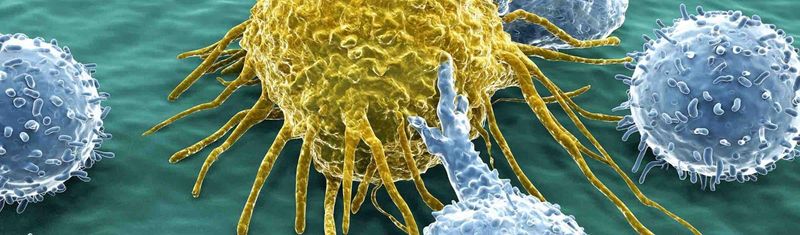
Frank: The SYNTHORIN platform has been an incredibly exciting addition to our cancer immunotherapy program because it enables our teams to design proteins that have unique molecular properties. In the case of IL-2, we are investigating how we can engineer the molecule to bind effectively to the part of its receptor responsible for expansion of cancer-fighting immune cells, while sparing the part that is responsible for side effects. That means we could potentially activate immune cells that are optimized for fighting cancer–such as killer T cells and Natural Killer (NK) cells–without the toxic side effects.
John: Building on what Frank described, we are also exploring the use of small molecule drugs to fight cancer while sparing normal tissues by designing monoclonal antibodies that carry a small, chemical drug directly to tumor cells. Antibody–Drug Conjugates can potentially bind to a protein expressed on different types of cancer cells, but not to normal cells. We are working on an antibody designed to carry a cytotoxic drug that attacks the cell-division machinery of tumor cells. This approach reduces collateral damage to healthy tissues while getting more of the chemical toxin into the cancer cells. Our teams are exploring this approach for treating lung cancer and other malignancies.

Sanofi technology platforms provide its R&D teams the tools they need to design pioneering therapeutics, and to understand biological pathways that connect many different diseases
How are Sanofi scientists approaching cell therapy?
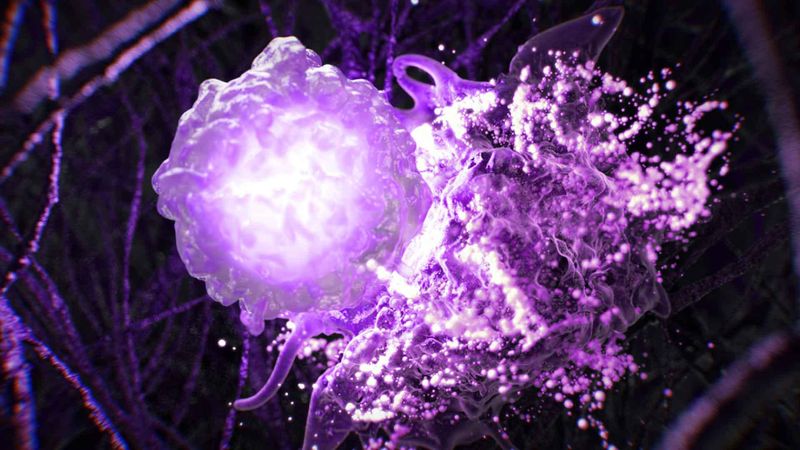
John: One of the latest frontiers in the battle against cancer is cell-based therapies, particularly chimeric antigen receptor (CAR)-T cell therapy. As practiced today, CAR-T-cell therapy entails extracting immune cells from a patient, genetically modifying them in the lab, and returning them to the patient where they can fight tumor cells. For patients with lymphoma and leukemias, this type of individualized cancer therapy has been quite successful, but it is often associated with significant side effects. Moreover, if the cell infusion fails to remove all cancer cells, successive treatments are generally not feasible.
Our teams are addressing these challenges by developing a novel cell-based cancer therapy using a platform pioneered by Kiadis, a biotech company we acquired recently. The Kiadis platform takes NK immune cells from volunteer donors whose genotype is optimized for cancer-fighting properties. These cells are expanded in the laboratory at industrial scale, so potentially, many patients could be treated based on a single donation. These donor-derived NK cells can also be genetically modified to express cancer-binding receptors, such as those used in CAR-T cell therapy.
This new, “universal” platform makes it possible to design NK cells for treating essentially any patient, which could avoid the need to generate individualized cell therapies. Many doses of these NK cells can be generated per batch, which makes it feasible to re-dose patients.
What other new technologies are changing cancer R&D?
Frank: Non-viral gene therapy is another exciting frontier because it allows us to deliver a piece of RNA or DNA to a specific type of cell in the body, where it provides instructions for changing that cell's function. Through our recent acquisition of Tidal Therapeutics, we now have access to an immune-cell-reprogramming technology that could revolutionize how we deliver future immunotherapy in patients. By using nanoparticles to deliver mRNA directly to specific types of cells, for example, it may soon be possible to reprogram killer T cells into CAR-T cells in the body.
Thus, we are working to fundamentally change how CAR-T cell therapy will be performed in the future. With this technology, we have the tools to create “off-the-shelf” mRNA therapeutics. That means we can explore ways to design and produce cell therapies on a large scale. This is so important because it means we could potentially boost a patient's ability to fight cancer in a much more convenient and cost-effective way.
What does this mean for the cancer community?
Frank: We can see the next wave in cancer immunotherapy on the horizon, hand in hand with a step change in molecular oncology. Both developments converge towards new, more targeted therapies that have a higher chance of achieving a durable remission in patients and a lower chance of causing side effects. That means a lot for the cancer community.
John: Beating cancer will take several complementary approaches. Our multi-faceted approach leverages new technologies to design innovative molecules, breaking the mold for oncology drug discovery. Taken together, our expanded toolkit, commitment to innovation, and culture of collaboration are enabling us to make real breakthroughs for people battling with cancer, and for their communities.